Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions or concerns about your health.
Most families hear about mesothelioma in commercials, not real life, so the early signs are easy to brush off. In fact, lifetime risk estimates show that about 1 in 220 men and 1 in 960 women born in 1961 in the UK will be diagnosed with mesothelioma, underscoring how common asbestos-related disease truly is. A nagging cough, a little fatigue, or “just age” can hide something more serious. The problem is that this cancer often develops slowly. By the time symptoms feel “bad enough,” it is already advanced. In the UK alone, about 2,700 new cases of mesothelioma are diagnosed each year, based on recent averages. Learning what to watch for and what not to ignore gives families a better chance to push for answers sooner. Below are warning signs many people overlook.
Shortness of breath

You expect to breathe harder after stairs or heavy lifting, but shortness of breath while talking, resting, or doing light chores may be due to mesothelioma. A loved one may describe pressure on one side, a band around the ribs, or air that “will not come in all the way.” When breathing feels wrong for weeks, and quick fixes do not help, it is vital to mention any asbestos exposure and ask the doctor to look beyond routine causes.
Chest or belly pain that quietly becomes routine
Early pain from asbestos disease is often dull and vague. A nagging ache under the ribs, along one side of the chest, or across the upper belly may come and go. People swallow pain pills and move on. Watch for pain that keeps returning to the same area, wakes someone at night, or gradually sharpens. Be sure to notice what makes it better or worse.
Also Read: How to Manage a Cold Feeling in Your Stomach
A lingering cough and hoarse voice

Coughs are easy to blame on smoking, seasonal allergies, or a lingering cold. With asbestos cancers or other severe lung conditions, however, a cough often lingers for weeks or months and does not improve with usual treatments. The cough may be dry or produce only a small amount of mucus, but its persistence is a key warning sign.
Hoarseness or a tired-sounding voice, especially in the evenings, can be another subtle but essential sign. If a cough has become part of your daily routine, it’s wise to ask a healthcare provider about a chest X-ray or CT scan, even if a physical exam seems normal. Imaging can detect significant changes in the lungs or chest that may not be apparent during a quick check-up.
Other signs to watch for include shortness of breath, unexplained fatigue, or mild chest discomfort. Keeping track of how long the cough has lasted, its severity, and any triggers can help clinicians identify the cause sooner and guide appropriate testing and treatment.
Weight loss and profound fatigue that you did not plan
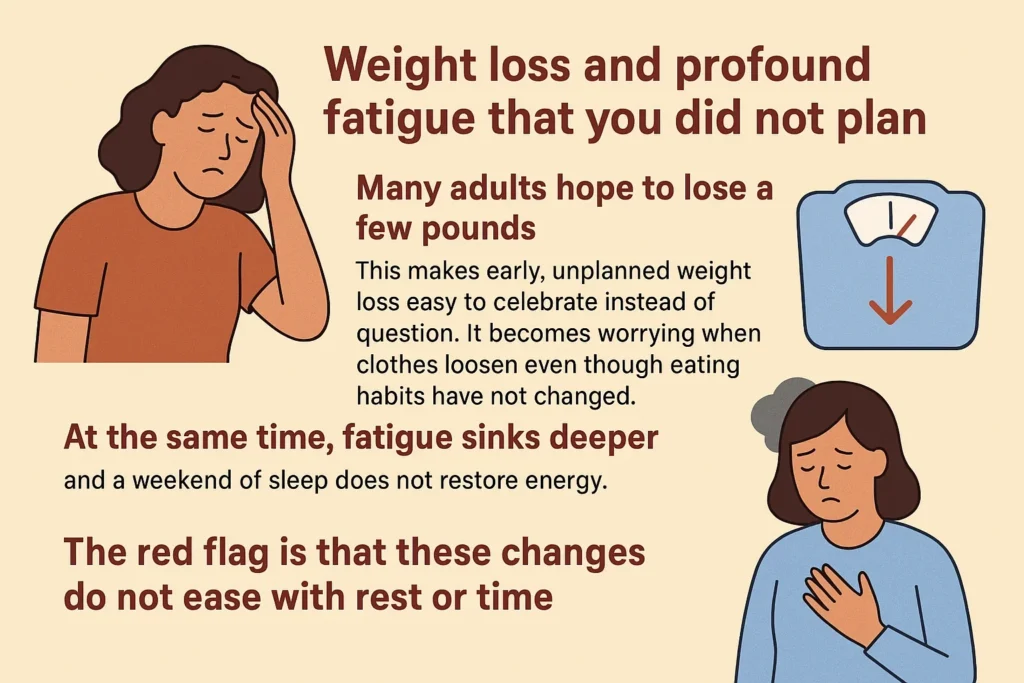
Many adults hope to lose a few pounds, so early, unplanned weight loss can be easy to celebrate rather than question. It becomes concerning when clothes start to feel loose even though eating habits and activity levels have not changed. At the same time, fatigue may deepen, leaving you drained even after a whole night’s sleep or a restful weekend.
The red flag is that these changes do not improve with rest or time. Other accompanying signs may include loss of appetite, night sweats, fevers, or persistent weakness. When weight loss and fatigue occur together without an obvious explanation, it is essential to discuss them with a healthcare provider. They may recommend basic blood tests, imaging, or other investigations to rule out underlying conditions such as infections, thyroid disorders, autoimmune diseases, or even malignancies.
Tracking the timing, amount of weight lost, and patterns of fatigue can help clinicians identify potential causes more quickly and guide timely intervention.
Also Read: What to Eat for Optimal Health: Top 10 Healthy Foods
Recurrent fluid buildup or frequent infections
Some people notice swelling or a sense of fullness in the chest from pleural effusions, while others may only discover the fluid incidentally on a chest X-ray or CT scan. You might also experience repeated bouts of pneumonia, stubborn colds, or lingering respiratory symptoms. Fevers may come and go, and changes in breath sounds, such as decreased or absent sounds over some regions of the lungs, can be clues.
It’s essential to ask about imaging if infections keep recurring. Clarify whether fluid was present, how much there was, and whether it returned after previous episodes or treatments. When fluid recurs, clinicians can perform diagnostic tests on the fluid, such as cytology, cultures, or chemical analysis, and may consider draining it to relieve symptoms. Identifying an underlying cause, such as heart failure, infection, autoimmune conditions, or malignancy, earlier can help guide treatment and prevent complications.
Endnote
Symptoms alone do not equal a diagnosis. Still, patterns point the way. Trust your notes and your instincts. Share work history, materials you handled, and buildings you lived in. Ask for imaging, and ask what each result means.
If concerns persist, request a referral to a center that treats rare cancers frequently. Early action improves choices, comfort, and peace of mind. Your attention today can buy time tomorrow, which is worth the effort.