Disclaimer: This article is for informational and educational purposes only and is not intended as medical advice. Athletes should consult a qualified healthcare or sports nutrition professional before making changes to their training, nutrition, or supplement routines.
Athletes rely on bone as a dynamic, living structure, not just a passive frame. Strong bones help tolerate training loads, transmit force efficiently, and reduce time lost to bone stress injuries. In practice, “bone health” is closely tied to training progression, fueling, sleep, and key nutrients that support normal mineral metabolism.
Bone Remodeling in Plain Language
Bone is always renewing itself by a process called remodeling. You have one set of cells that make new bone (formation) and another that breaks down old bone (resorption). This cycle is healthy and essential: It repairs micro-damage, adjusts to training, and maintains structure. In the case of stress during training, remodeling activity can also increase and remain elevated.
If the resources of recovery are sufficient, bone formation continues at a corresponding rate and the skeleton models. If recovery is incomplete, particularly with reduced energy intake, resorption may exceed formation for longer durations than before, and the response may be attenuated.
What Bone Mineral Density Means
Bone mineral density (BMD) describes how much mineral content is packed into bone tissue. Higher BMD generally correlates with greater bone strength, but it is not the only factor. Bone geometry, microarchitecture, and sport-specific loading patterns also affect fracture risk and performance capacity.
For athletes, BMD matters because it can influence tolerance to repetitive impact (running) or high force outputs (jumping, Olympic lifts). Low BMD can be a red flag, particularly in athletes with recurrent bone stress symptoms, a history of stress fractures, or prolonged periods of under-fueling.
Common Athlete Risks for Lower Bone Resilience
Several athlete scenarios raise risk:
- Low energy availability from chronic under-eating or aggressive weight cuts
- Rapid increases in running mileage, sprint volume, or jump counts
- Indoor-heavy training blocks and winter seasons with minimal sun exposure
- High training monotony with limited recovery days
- Endurance athletes and weight-class athletes with long stretches of restricted intake
These factors do not guarantee injury, but they increase the importance of fundamentals: progressive loading, strength training, and nutrition that supports remodeling.
Also Read: Nutrition, Activity & Culture: Modern Wellness in Traditional Places
Vitamin D3 for Athletes: Bone and Muscle Support
Vitamin D3 plays a central role in calcium absorption and mineral balance, both of which matter for bone mineralization. It also supports normal muscle function, which can indirectly affect injury risk by altering movement quality, fatigue resistance, and training tolerance.
Also Read: Hyperbaric Chamber Muscle Recovery Benefits & Athletic Performance Impact
Why Vitamin D Status Often Runs Low in Sport
Vitamin D deficiency is common in the general population. It can also be common among athletes, especially those who train indoors, live at higher latitudes, cover skin due to the climate, or spend most of their training hours early in the morning or late in the evening. Winter seasons can be a particular challenge because sun exposure drops while training demands may remain high.
Evidence from elite sport populations reinforces how widespread this issue is. Studies have shown that among professional basketball players, 32% were vitamin D deficient and 47% had insufficiency. Among National Football League (NFL) athletes, 26% lacked vitamin D, while 42% to 80% exhibited insufficient vitamin D levels. Similarly, assessments of Liverpool’s professional football players found that 36% had either deficiency or insufficiency.
Vitamin D and Bone Stress Injuries: Association vs Causation
Low vitamin D status is commonly implicated in the sports nutrition literature and observational studies as an increased risk factor for bone stress injury development including stress fractures. But association is not proof of low vitamin D by itself causing the injuries. Bone stress injuries are multifactorial and typically occur as a result of errors in training load, poor energy availability, inadequate strength training, lack of sleep, and individual biomechanics.
But despite that fine print, getting enough vitamin D is considered in the athletic world a fundamental step for health — since it helps with normal calcium absorption and bone mineralization.
How Athletes Typically Assess Vitamin D
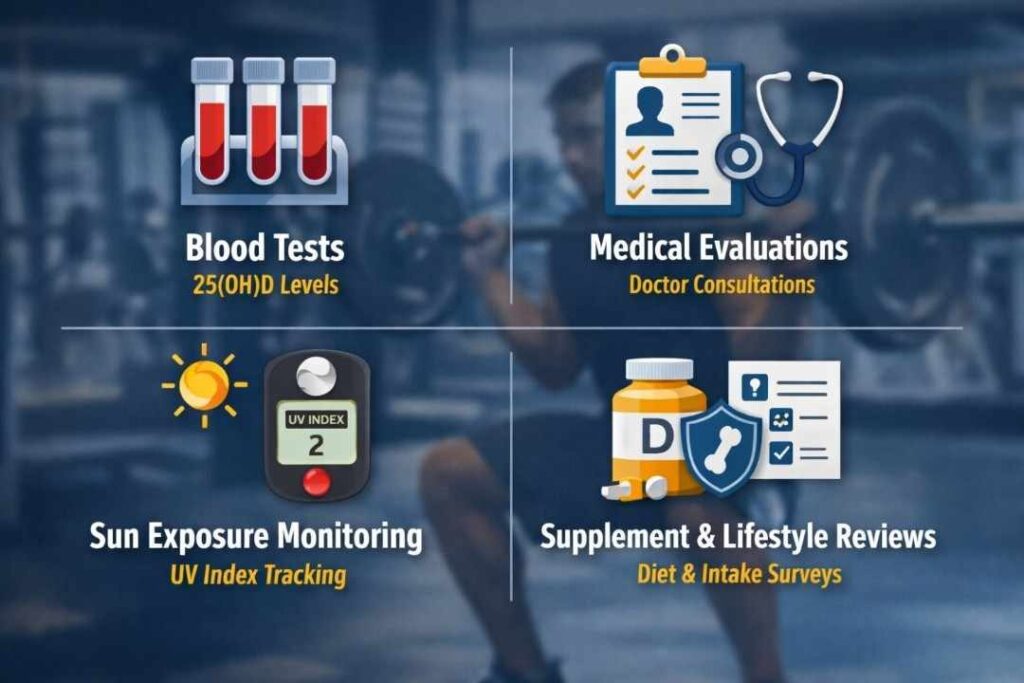
In the clinic, blood testing is frequently used to monitor vitamin D status. This is not uncommon among athletes with repeated stress-related injuries, intractable bone pain, or prolonged indoor training. Testing will also prevent a lot of speculation and allow all decisions to be made according to one’s status, rather than on guesswork.
Vitamin K2 and Bone Metabolism: Calcium Handling Made Simple
Vitamin K2 is best thought of as a “calcium-handling” vitamin. It is essential to promote the activation of certain vitamin K-dependent proteins associated with mineralization metabolism and bone physiopathology. Instead of “adding calcium,” K2 is explained as enabling the body to properly use calcium within normal biological processes.
What K2 Might Do in a Practical Athlete Context
Put simply, VKD proteins are involved in pathways that channel calcium to mineralized tissues (bone). It is one reason K2 is sometimes conceptually combined with vitamin D, a nutrient that also supports calcium absorption. Those seeking long-term bone resilience might consider K2 as a potential player in the broad panorama of micronutrients targeted for athletes.
What’s Known vs Uncertain About K2 Supplementation in Athletes
General bone health discussions are more established in K2 research than in athlete-specific injury prevention. In non-athlete populations, some clinical trials and systematic reviews reported effects of K2 supplementation on changes in bone-related biomarkers or bone measures; however, direct evidence on whether K2 supplementation effectively reduces the occurrence of athletic injuries remains limited. In athletes, the outcome depends significantly on training periodization, energy availability, and strength work, thereby preventing the determination of only the K2-effect.
Shilajit Overview: What It Is and How Athletes Use It
Shilajit is a natural substance formed over long periods by the decomposition of plant matter and microbial processes, typically found in mountainous regions. It is commonly described as containing fulvic acids and a spectrum of trace minerals, though composition can vary depending on origin and processing.
From an athlete’s perspective, shilajit is often used as a “training support” supplement, more about supporting day-to-day recovery capacity and consistency than about targeting a single tissue. Compared with vitamin D, evidence is more established for vitamin D’s role in bone outcomes. In contrast, the direct effects of shilajit on bone density in athletes are less well-defined in the research literature.
Some athletes encounter shilajit resin products labeled Shilajit Live Resin (for example, Pürblack Shilajit Live Resins), reflecting one naming format used for shilajit preparations.
Bone Density and Injury Prevention: What Supplements Can and Cannot Do
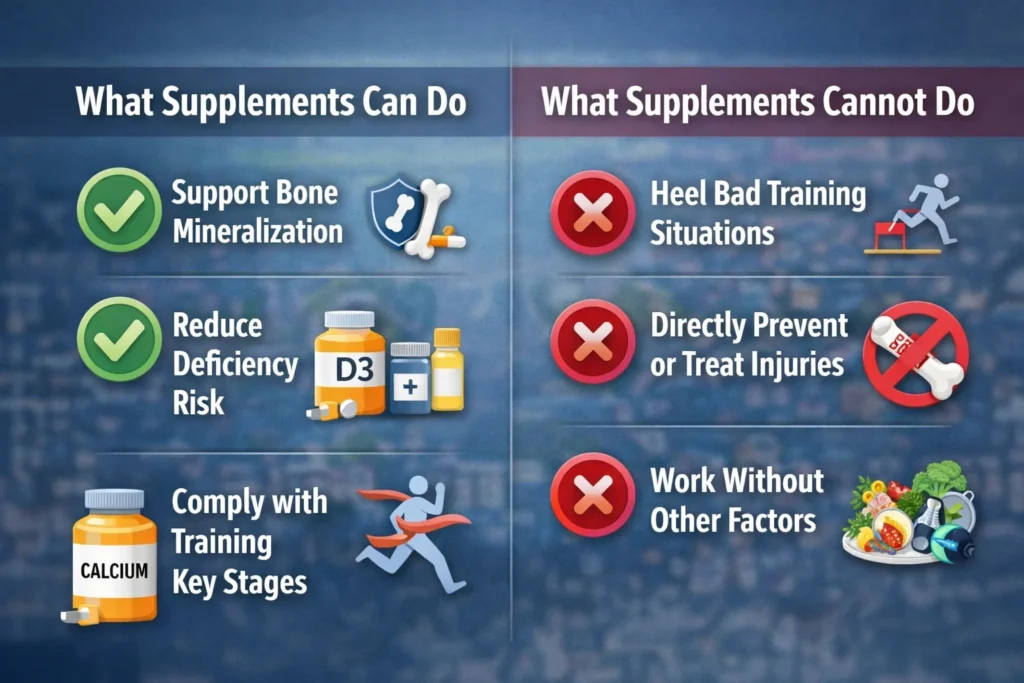
Supplements can support physiology, but they cannot replace the fundamentals that drive bone adaptation. Bone responds to progressive mechanical loading over time, which is why structured strength training and gradual increases in impact volume are central to bone resilience. Sleep and recovery are not optional extras; they influence the hormonal and metabolic environment that determines whether remodeling supports adaptation or drifts toward breakdown.
Nutrition is equally foundational. Adequate energy availability is critical for normal bone turnover, and protein supports the musculoskeletal system broadly. When athletes under-fuel for long periods, bone remodeling can shift in an unfavorable direction, increasing the risk of stress injuries, particularly during high-volume phases.
It also helps to set realistic timelines. Bone density changes are not immediate; measurable shifts typically take time and depend on consistent loading and adequate nutrition. Injury risk is multifactorial, so even “good” nutrients do not guarantee protection if training spikes, recovery is poor, or fueling is inadequate.
Practical Athlete-Focused Takeaways
- Consider periodic screening for vitamin D status during winter, long indoor blocks, or after recurring bone stress symptoms.
- Treat vitamin D3 as foundational for calcium absorption and normal mineral metabolism, especially when status is low.
- View vitamin K2 as a possible “supporting player” in calcium handling, while recognizing athlete-specific outcomes remain uncertain.
- Use shilajit as a general training-support option rather than expecting rapid or guaranteed changes in bone density.
- Pair any supplement plan with progressive training, strength work, adequate energy intake, and consistent sleep.
- If you take medications or manage a medical condition, discuss supplements with a qualified clinician to avoid unwanted interactions.
For athletes focused on bone density and injury prevention, vitamin D3 has the most apparent connection to bone physiology, as it affects calcium absorption and mineral balance. Vitamin K2 is involved in vitamin K-dependent proteins involved in calcium handling, but the relationship to athletic injury outcomes is not firmly established. Shilajit is widely used in sports as a general support supplement and may fit best within a long-term routine aimed at consistency and recovery, while recognizing that direct evidence for bone density outcomes is less developed than for vitamin D.